
‘Aging with grace’: The next big challenge for urbanists
In late October, experts gathered in Seaside, Florida, to confront one of the greatest demographic issues of our times: the aging of the American population. With the Baby Boom soon to become the Elder Boom, Seaside founder Robert Davis concluded that New Urbanists should be figuring out how the country can best navigate the massive age shift now under way.
Many of New Urbanism’s leaders and originators have entered or will soon reach retirement age (though few of the ones I know have stopped working). Davis, who began developing his 80-acre resort town in the early 1980s, will turn 75 on Nov. 10.
Looking at what’s been happening at Seaside and elsewhere, Davis decided to have the Seaside Institute’s program director—Washington, DC, architect Dhiru Thadani—organize a two-day symposium on “Aging with Grace,” attended by about 55 people mainly from the Southeastern states. Thadani brought together more than a dozen speakers with extensive backgrounds in public health, architecture, planning, “wellness,” and other fields.
Andres Duany, 68, got the conclave under way by distinguishing between two periods of later life. One, Duany said, is “old age,” which in its initial years, when people still possess considerable energy, “has its comforts.” The other is “old old age,” a later period often marked by substantial decline and fragility.
Duany said that as they age, some people will need features such as orange doorknobs (because they have trouble seeing) or raised dishwashers (because they have trouble bending over). But, he said, many baby boomers will insist, for as long as possible, on seeing themselves as vital individuals who “really enjoy life.” They will not respond well to overt marketing of features that bring to mind deterioration and decline.
That aging is a very sensitive topic is borne out by the experience of Worman’s Mill, a 307-acre development in Frederick, Maryland. Since 1988, the Wormald Companies, a family-owned building firm, has been constructing the 1,497-unit community on a former farm three miles north of Frederick’s downtown.
Roughly half the Worman’s Mill residents are 55 or older, yet only once—in an early stage—did the company advertise the development as a “retirement community.” “That was a huge mistake,” said Robert K. Wormald, a managing partner in the company. It made many people, especially younger ones, reluctant to come and buy homes. Consequently, for most of its three decades of construction, Worman’s Mill has adhered to less explicitly age-related descriptions of what’s on offer.
Advertising has emphasized first-floor master suites (popular with older couples), maintenance-free exteriors, and the fact that outdoor tasks like lawn-mowing are not the responsibility of the residents; those chores are handled by the community association. Sales staff extol a “lock-and-go” lifestyle (popular with retirees who travel frequently). This strategy appeals to seniors, without directly talking about age.
The symposium suggested that if “aging with grace” is become a widespread aim, it’s one that will have to be presented very discreetly to the younger portion of the intended market. For the “old old,” on the other hand, the afflictions that aging eventually brings are not something that can be left undiscussed. A major challenge, many speakers averred, will be how to protect fragile individuals (many of them in their eighties and nineties) from a “medical-industrial complex” that prescribes too many pills and keeps too many people tied to tubes after the time for such aggressive treatment has passed.
What the numbers say
Speakers with backgrounds in public health, architecture, planning, “wellness,” and other fields presented a sometimes startling array of statistics:
- Each day, another 11,509 Americans turn 65.
- By 2030, between 25 and 27 percent of the population will be 65 or older.
- By 2035, there will be more Americans 65 and older than there will be children under age 18.
- Nationally, the fastest-growing group is people who have been on the planet for eight decades or more.
- Zero percent of Americans want to end their days in a nursing home. But 33 percent are likely to spend time there, and 24 percent will stay for more than six months.
- The average nursing home resident receives only four visitors a month, said Dr. John McGinty, a consultant to hospitals across the country.
- The average life span is 79 years, said Dr. Hillary Glenn, co-founder of the Point Washington Medical Clinic in Santa Rosa Beach, Florida. But the average “health span”—the period of being largely unhampered by disease and ailments—is considerably shorter: 63 years.
Housing and transportation are major concerns. “Our housing is built for able-bodied 35-year-olds,” said Leslie Spencer of AARP’s Florida office. Since the 1920s, communities and roadways have been built predominantly for automobiles. It’s often not easy to find cafes, parks, and other gathering places within walking distance.
The website SeniorLiving.org touts the advantages of “continuing-care retirement communities” (CCRSs), which offer a combination of independent living, assisted living, and nursing home. SeniorLiving.org says that for people with financial means, a CCRC “may be the ideal senior living option to ‘age in place.”
Sometimes that may be the case. But if a CCRC is not physically connected to a walkable town or neighborhood center, can it really be ideal? Dr. Richard Jackson, professor emeritus at UCLA’s Fielding School of Public Health, recalled talking with a retirement community resident who felt frustrated by his surroundings. “I can’t go for an interesting walk without getting on a jitney,” the man lamented.
Depression does not necessarily escalate with age, Jackson said, but “having certain chronic conditions or being isolated increases the risk. This is why keeping chronic conditions at bay [such as arthritis or limited vision whenever possible] and staying engaged are so important.”
Building more wisely
A sensible overall response to aging might be the more or less standard New Urbanist recipe: Develop communities that bring housing, stores, restaurants, offices, and other elements of daily life into close proximity. Place small parks throughout the community, connected to people’s homes by an inviting street and sidewalk network. Create a mix of sizes and types of housing so that people can stay in a community through every stage of life.
Worman’s Mill tries to achieve many of those goals. In the late 1980s, when Robert K. Wormald Sr. was leading the firm, he collaborated with David B. Wolfe, a marketing whiz who had a great feel for community life and well-being. The hypothesis of Wolfe, author of books such as Serving the Ageless Market, was that the elderly—even those in assisted living—would be happier if their housing complex were in a townlike setting.

Three decades later—and seven years after Wolfe’s death at 78—his vision is coming to fruition in the Worman’s Mill Village Center, the final element of the development. Now under construction, and scheduled for completion in 2019, the Village Center will have 171 apartments.
Some of the apartments will be in the second and third floors of a building that will contain retail businesses at street level. Some units will be restricted to people 55 and older, others to people 62 and up. All will be near three restaurants, a bakery, a nail salon, and an investment office. A convenience store will include a deli that will make sandwiches to order and will have tables where people can sit. The Village Center will have places to gather. “The Village Center has always been envisioned as intergenerational,” said Edward Wormald, a managing partner who is overseeing its development. “Within walking distance of the center will be 5,000 people,” said his brother, Robert Wormald.
The final element will be an assisted-living facility—though the development company avoids using that term. In it will be 69 units for individuals who need daily nursing care but who, at least in their better moments, will be able to circulate through the Village Center.
Operated by Sage, of the Philadelphia area, it is designed to resemble a hotel and to offer some hotel-like services. “There will be a happy hour at least weekly,” Edward Wormald noted. The four-story building also will contain rooms for 20 “memory-care” patients—individuals with Alzheimer’s Disease or other forms of dementia.
The hope, said Robert Wormald, is that that as a result of the Sage-operated facility, people who have lived in Worman’s Mill for years will be able to stay in the community, even after fully independent living has become impossible for them. They will be near their friends, and can be visited by them every day.
It’s worth noting that the 171 Village Center apartments also will be set up to accommodate people who need some assistance. Residents can obtain whatever services they require—hair-dressing, help with medications, dishwashing, cleaning, shopping, dog-walking. They will pay for their services a la carte. That’s much less expensive than moving to “assisted-living facilities with huge entry fees and huge rents,” Robert Wormald said.
Humanizing intimidating institutions
If the average nursing home resident gets only four visitors a month, and even those visits don’t last long, as Dr. McGinty said, part of the reason may be the off-putting character of most nursing homes. “Nobody wants to be there or to visit a nursing home,” said McGinty, a part-time Seaside resident who led hospitals in Kenosha, Wisconsin, and Columbus, Indiana, before launching a healthcare consulting firm.
Duany offered a design proposal that could take some of the curse off the nursing home: Break down its scale and make the institution appear more home-like. Duany showed sketches of that his firm, DPZ, generated in 2009 for an Atlanta Regional Commission initiative on “Lifelong Communities.”

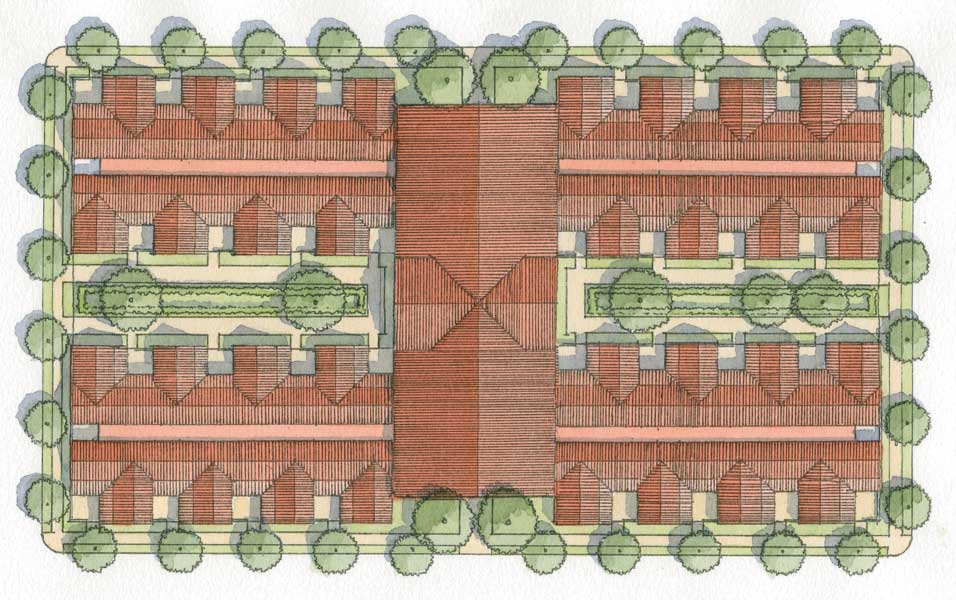
The sketches depicted a nursing home whose perimeter is made up of diminutive, connected cottages. They look like tiny dwellings straight out of the 19thcentury—“cute” in the extreme, Duany said. Each cottage contains a living room with a tiny kitchen, a bedroom, and a bathroom, plus a small courtyard garden.
A visitor, instead of having to enter the nursing home through an institutional lobby, would walk through a little garden gate and knock on the door of an individual cottage. The unit’s relatively domestic feel might overcome the resistance of visitors and patients alike. The cottages would be arranged side by side, like townhouses. At the rear of each row would be a wide corridor that the staff, from the main building, would use to enter each cottage and provide services.
Helping people stay at home
But many elderly would prefer to remain in their own homes as long as possible, Robert Davis pointed out. One of the things that enables people to do that is service providers who make house calls. A pioneer in providing such services is Beacon Hill Village, a nonprofit, locally based organization that was formed in 2002 to help senior continue to live in the tall, old, red brick houses and apartment buildings of Boston’s Beacon Hill.

More than 200 such neighborhood- or locally-based volunteer groups have sprung up around the nation in the past 16 years, and an additional 150-plus are in development. They’re in 45 states and the District of Columbia, says the Village to Village Network, a national organization that helps them get established.
“Yearly membership dues average about $450 nationally, and most villages offer subsidies for people who cannot afford membership costs,” The New York Times reported four years ago. “Armies of volunteers, who help run many villages, also help lower member costs by doing yard work, picking up prescriptions or taking members shopping or to the airport.”
Neighbors engage neighbors, alleviating the isolation that becomes troublesome as people get older and lose family members and longtime friends. The press sometimes calls them “virtual villages,” but that doesn’t sound quite right. People end up having face-to-face conversations and getting to know individuals who live, in many cases, not far away. They’re meant to function as communities. One participant observed that a village “gives you a sense of worth and accomplishment.”
As Robert Davis sees it, the residents of Beacon Hill formed their village organization “so they could live out their lives where they know their neighbors.” It’s an alternative to becoming uprooted by moving to a geographically remote retirement community.
Last summer Robert Davis began talking with Susan Davis (no relation), who had headed the Sacred Hearth Health System in Pensacola, Florida, about establishing a source of services for older residents of communities along State Rt. 30A, including Seaside and nearby Rosemary Beach. “There is such fragmentation of services, and you have to be knowledgeable about how to access them,” Susan Davis told me.
The organization that Robert Davis and Susan Davis are contemplating would help guide people through the thicket of what’s available. Services could be “integrated with a wellness program, diet, exercise, meditation, entertainment, and education,” the Seaside developer said.
What can an individual do?
The symposium took encouragement from AARP’s growing interest in walkable communities. Said Dhiru Thadani: “AARP is now taking the lead on the issues that New Urbanists were talking about.”
Part of the symposium headed into a more personal realm: How individuals can improve their own health and well-being, never mind where they live. Dr. Hillary Glenn observed that many diseases of aging are really diseases of chronic inflammation. In her own case, she was told by physicians that her severe rheumatoid arthritis could be fought with infusions—six a year at $36,000 apiece.
“I couldn’t afford that,” Glenn said. “The country can’t afford that. Therefore she looked at lower-cost, more natural methods, such as yoga and Tai Chi. She found that “95 percent of all illnesses are caused or worsened by stress.” Learning to actively relax became a priority. She came to see food as something that can activate a painful genetic predisposition or turn those genetic influences off.
Elizabeth Trapp, a registered dietitian, castigated the “standard American diet” and urged people to shift to a plant-based diet high in fiber and phytonutrients.” She told of positive results from an “anti-inflammation diet.” Dr. C. Jon Raley, a chiropractic doctor in Andalusia, Alabama, urged everyone to sit less because excessive sitting causes or exacerbates physical problems and is harmful to the brain as well.
Marie Boularand, naturopath, psycho-bio therapist, and founder of the Biodecoding Institute, argued that “diseases are logical and intelligent.” By her reckoning, a disease is the body’s way of responding to “a past trauma that we failed to heal.” Delve deeper to identify the buried trauma and resolve it, and the disease may vanish, she suggested. “The symptom is the roadmap to healing ourselves.”
Dr. Prudence Farrow Bruns, a teacher of Transcendental Meditation, said the baby boomers grew up in “a very difficult time”—during the Cold War and after two world wars and the development of the hydrogen bomb–so it’s not surprising that they had a quest for self-expression and were “not going to go the way the world told us.” This propelled some to undertake an inward search, said Bruns. Here own search sent her to India to study with Maharishi Mahesh Yogi, and led John Lennon, who was doing the same, to write the Beatles song “Dear Prudence.”
Bruns praised TM for having “a balancing effect on the busy mind,” observing, “If you can be quiet and still, … you can be in control,” she said. As evidence of TM’s effectiveness, she showed a chart indicating that those who started practicing TM by age 65 saw their spending on physicians go down, while those who didn’t practice TM saw their use of doctors, and their spending on doctors, rise. “There was a remarkable drop in expenses for those in TM.”
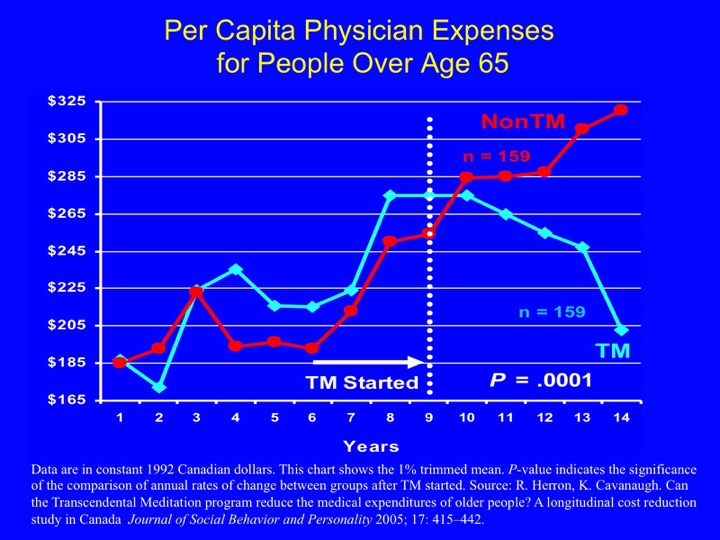
A second chart tracked a decline in stroke, heart attack, and death among people who practiced TM. “When we talk about aging gracefully,” Bruns proposed, “it is a mental state.”
At symposium’s end, it was up to each participant to sort through the 13 presenters’ disparate ideas about aging and reach their own conclusions. Whatever particular argument one agreed with or dissented from, the overall thrust of the program was clear: aging gracefully is something each individual can aim for, but the search will go better if you’re part of a community.




